More Than Just "Faking It"
Picture this: A 35-year-old patient walks into the emergency room for the fourth time this month, clutching their abdomen and describing excruciating pain. Their medical history reads like a mystery novel—multiple surgeries, countless specialist visits, and a collection of diagnoses that don't quite connect. The attending physician exchanges a knowing glance with the nurse. Something doesn't add up, but what exactly is happening here?
This scenario plays out in hospitals across the country every day, presenting healthcare providers with a complex puzzle. Is this person genuinely suffering from an undiagnosed condition? Are they driven by a deep psychological need to be sick? Or are they deliberately deceiving medical professionals for personal gain?
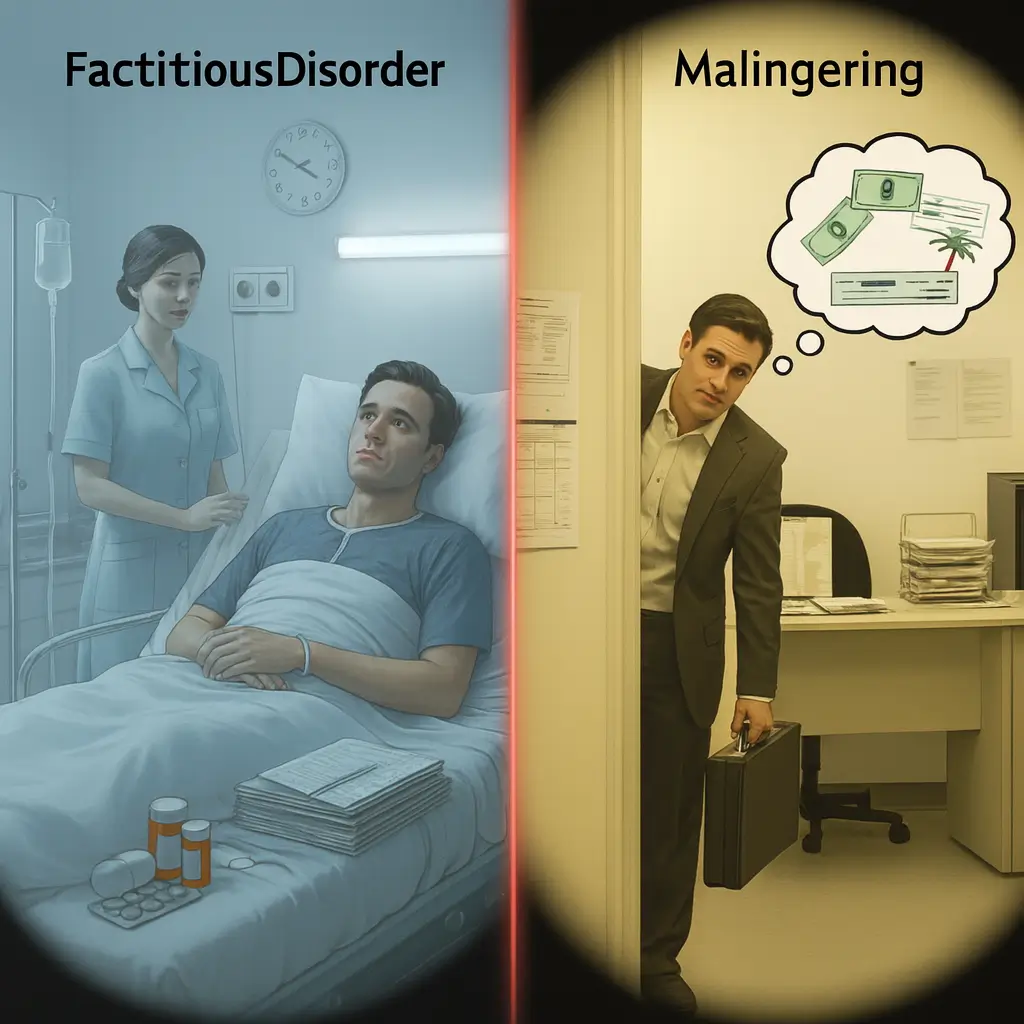
The answers lie in understanding two distinct but often confused conditions: factitious disorder and malingering. While both involve the fabrication or exaggeration of symptoms, their underlying motivations couldn't be more different. One stems from a genuine mental health condition that compels individuals to seek the "sick role," while the other represents a calculated deception aimed at achieving specific external benefits.
This article will clarify the crucial distinctions between factitious disorder and malingering, explore their signs and symptoms, examine the diagnostic challenges healthcare providers face, and outline potential treatment approaches. Understanding these differences isn't just academic—it's essential for ensuring patients receive appropriate care while protecting the integrity of our healthcare system.
It is alo important to know that these deiseases fall into a class of Somatoform disorders, which are a group of mental health conditions characterized by physical symptoms that are not caused by any underlying medical condition. If you would lke to dive deeper into the understanding of this on a medical level this video is very helpful.
What is Factitious Disorder? The Need to Be Sick
Factitious disorder represents one of the most perplexing conditions in mental health. Individuals with this serious psychological disorder deliberately produce, fake, or exaggerate symptoms to assume the role of a patient. Previously known as Munchausen syndrome, this condition goes far beyond simple attention-seeking behavior.
The primary motivation driving factitious disorder is internal—a powerful psychological need for the attention, sympathy, and care that comes with being sick. Unlike malingering, there's no obvious external reward driving the behavior. Instead, these individuals find emotional fulfillment in the medical attention they receive, the concern shown by healthcare providers, and the identity of being a patient.
At Prescott House, we've encountered individuals whose substance abuse issues intertwined with factitious behaviors, creating complex treatment scenarios that required careful unraveling of motivations and underlying psychological needs.
Common behaviors associated with factitious disorder include exaggerating existing symptoms or lying about new ones entirely. More concerning, some individuals intentionally harm themselves to create authentic symptoms—injecting bacteria to cause infections, inducing seizures, or creating wounds that won't heal. They may tamper with medical tests, contaminating urine samples or manipulating thermometers to suggest fever.
These individuals often possess extensive knowledge of medical terminology and diseases, allowing them to present convincing symptom narratives. They typically have histories of seeking treatment at numerous hospitals, sometimes using fake names or identities to avoid detection. Perhaps most alarming, they often eagerly agree to risky surgeries or invasive procedures that others would naturally avoid.
A particularly troubling variant is Factitious Disorder Imposed on Another (FDIA), formerly known as Munchausen syndrome by proxy. In these cases, a person—often a caregiver—falsifies or deliberately induces illness in someone under their care, typically a child. This form represents one of the most serious manifestations of the disorder, as it directly endangers vulnerable individuals.
Understanding Malingering: Deception with Purpose
Malingering sits on the opposite end of the spectrum from factitious disorder, though the surface behaviors may appear remarkably similar. Where factitious disorder stems from internal psychological drives, malingering is fundamentally about external gain. It's a conscious, deliberate choice to fake or exaggerate illness symptoms to achieve specific, tangible benefits.
The key distinction lies in motivation and awareness. Individuals who malinger are fully aware of their deception and have clear reasons for it. They might fake back pain to avoid returning to a job they dislike, exaggerate PTSD symptoms to increase disability benefits, or claim ongoing injuries to prolong workers' compensation claims. The "illness" serves as a tool to achieve something concrete and valuable.
Common scenarios for malingering include workplace injuries where continued symptoms mean continued time off work or financial compensation. We see this in legal contexts too, where individuals might exaggerate mental health symptoms or cognitive impairments to influence court proceedings or avoid criminal responsibility. Military personnel might malinger to avoid deployment, while students could fake learning disabilities to gain academic accommodations.
In addiction treatment settings, malingering can be particularly complex. At Prescott House, we've observed cases where individuals exaggerated mental health symptoms to gain access to certain medications, or fabricated trauma histories to justify their substance use. These situations require careful assessment to distinguish genuine co-occurring disorders from manipulative behaviors designed to deflect from addiction treatment.
Unlike factitious disorder, malingering often has an endpoint. Once the desired goal is achieved—the insurance settlement is received, the court case is resolved, or the unwanted work assignment is avoided—the symptoms typically disappear. This pattern of symptom resolution coinciding with goal achievement often provides crucial diagnostic clues for healthcare providers.
Malingering behaviors tend to be less elaborate and medically sophisticated than those seen in factitious disorder. Where someone with factitious disorder might study medical texts to present convincing symptom combinations, a malingering individual typically focuses on symptoms that are difficult to objectively verify—pain, fatigue, memory problems, or emotional distress.
Key Differences: Side-by-Side Comparison
Understanding the distinctions between factitious disorder and malingering requires examining several crucial factors that differentiate these conditions.
Motivation and Awareness
The most fundamental difference lies in why these behaviors occur. Factitious disorder is driven by an unconscious psychological need to occupy the patient role—these individuals genuinely don't understand why they feel compelled to fake illness. Malingering, conversely, involves conscious deception for clear external benefits. The person knows exactly why they're faking symptoms and what they hope to gain.
Medical Knowledge and Presentation
Individuals with factitious disorder often display impressive medical knowledge, presenting complex symptom patterns that initially fool healthcare providers. They may have extensive medical histories across multiple healthcare systems. Malingering individuals typically focus on subjective symptoms that are harder to verify medically—they're not trying to impress doctors with medical knowledge, just convince them of their inability to function normally.
Response to Treatment
Those with factitious disorder often welcome medical interventions, even painful or risky procedures, because medical attention fulfills their psychological needs. They may appear to improve temporarily but then develop new symptoms or complications. Malingering individuals tend to be more selective, showing little improvement with treatment until their external goals are met, at which point symptoms may resolve surprisingly quickly.
Healthcare Seeking Patterns
Factitious disorder typically involves extensive healthcare utilization across multiple providers and systems. These individuals often travel between hospitals and use different identities to avoid detection. Malingering usually involves more targeted healthcare seeking, focused on specific providers or institutions that can provide the needed documentation or benefits.
Duration and Persistence
Factitious disorder tends to be chronic and persistent, with individuals continuing to seek medical attention even when it's clearly not in their best interest. Malingering often has a more defined timeline, ending when the external goal is achieved or no longer attainable.
Diagnostic Challenges for Healthcare Providers
Identifying these conditions presents significant challenges for healthcare professionals. The primary difficulty lies in distinguishing genuine medical conditions from fabricated ones while maintaining the therapeutic relationship necessary for effective care.
Healthcare providers must walk a careful line between healthy skepticism and maintaining trust with patients who may genuinely need help. Premature accusations of faking illness can destroy therapeutic relationships and potentially endanger patients with real but difficult-to-diagnose conditions. Yet, failing to identify factitious disorder or malingering can lead to unnecessary procedures, wasted resources, and continued enablement of harmful behaviors.
Red flags that might suggest factitious disorder include extensive medical histories with unclear diagnoses, symptoms that don't follow typical disease patterns, resistance to discharge from hospitals, unusual complications following procedures, and evidence of self-harm or symptom production. The presence of medical knowledge that seems inconsistent with the person's background, or a pattern of seeking care at multiple institutions, can also raise suspicions.
For malingering, warning signs include symptoms that conveniently align with external incentives, inconsistencies between reported symptoms and observed behavior, lack of cooperation with diagnostic procedures, and symptoms that improve or worsen in correlation with external circumstances rather than medical interventions.
Moving Forward: Hope Through Understanding
The distinction between factitious disorder and malingering extends far beyond academic classification—it represents the difference between a cry for help and a calculated deception. Understanding this difference is crucial for healthcare providers, families, and the individuals themselves who may be trapped in these complex behavioral patterns.
Factitious disorder emerges from deep psychological wounds that drive individuals to seek comfort and attention through the medical system. These individuals aren't simply "attention-seeking"—they're suffering from a genuine mental health condition that compels them to find identity and emotional fulfillment through illness. Their behaviors, while harmful, stem from an unconscious need that they often don't fully understand themselves.
Malingering, while equally challenging to address, represents a conscious choice made to achieve specific external goals. While this behavior can be frustrating for healthcare providers and costly for the system, it's important to remember that it often indicates underlying problems—financial desperation, job dissatisfaction, or other life stressors that drive individuals to see deception as their only option.
Both conditions highlight the complex relationship between mental health, physical symptoms, and the healthcare system. They remind us that healing requires more than just treating surface symptoms—it demands understanding the whole person and addressing the underlying factors that drive their behaviors.
At Prescott House, we've learned that these conditions rarely exist in isolation. They often intertwine with substance abuse, trauma histories, and other mental health challenges, creating intricate webs that require patience, expertise, and compassion to untangle. Recovery becomes possible when we approach these individuals with curiosity rather than judgment, seeking to understand rather than simply to diagnose.
If you recognize these patterns in yourself or a loved one, know that help is available. Both factitious disorder and the underlying issues that drive malingering can be addressed with appropriate treatment and support. The first step is often the hardest—acknowledging that there's a problem and being willing to explore the real needs driving these behaviors.
Whether you're struggling with compulsive illness behaviors, using deception as a coping mechanism, or dealing with co-occurring substance abuse issues, professional help can provide the tools and insights needed for genuine healing. At Prescott House, we understand that recovery isn't just about stopping harmful behaviors—it's about building a life that feels meaningful and fulfilling without the need for deception or self-harm.
Recovery is possible, and understanding is the first step toward healing. If you or someone you love needs support navigating these complex challenges, don't hesitate to reach out. Every journey toward wellness begins with a single, courageous step forward.















